Sperm Retrieval Procedures in Los Angeles & San Francisco, CA

State-of-the-Art Sperm Retrieval with Dr. Paul Turek
When a man hears from a doctor that he is infertile and sterile, he may understandably assume that he is out of options for becoming a biological father. In reality, most sterile men have viable sperm somewhere in the male reproductive tract that can be used to fertilize an egg.
Sperm retrieval is a process that carefully harvests this sperm so that it can be used to achieve pregnancy with assisted reproductive technology. It is a valuable tool for men with azoospermia (i.e., no sperm in the ejaculate) or who cannot ejaculate at all.
Dr. Paul Turek is an internationally renowned male reproductive surgeon who has focused his career on the complexity of sperm retrieval and has developed innovative techniques for finding and collecting hidden sperm. Having performed thousands of sperm retrieval procedures, he is uniquely qualified to help men who have been told they are infertile or sterile.
When Does Dr. Turek Suggest Sperm Retrieval?

Sperm retrieval is a good solution for men who either cannot ejaculate or have little to no sperm in their semen. To get around this problem, Dr. Turek can, in many cases, pull live, viable sperm from the male reproductive tract. The extracted sperm can then be used with an assisted fertilization procedures.
How Is Sperm Used After Retrieval?
Sperm that has been retrieved is generally considered “immature.” While it still contains the proper genetic material necessary to make a baby, the sperm itself may not have ability to move (motility) that is necessary to penetrate and fertilize an egg on its own. Therefore, the best way to achieve a pregnancy with retrieved sperm is by using fertilization procedures that include:
In Vitro Fertilization: IVF is a process that retrieves multiple eggs from a woman. These eggs are then fertilized with the sperm in a controlled laboratory setting. Eggs that have been successfully fertilized (now embryos) are then reimplanted in the uterus for the woman to carry the pregnancy.
Intracytoplasmic Sperm Injection: ICSI is an “add on” procedure used along with IVF. With IVF, sperm and eggs are bathed together in a dish and the best sperm fertilizes the egg. ICSI is an extra technique in which a single sperm is injected directly into the egg to increase the chances of fertilization. It is a great solution for men who have sperm found via sperm retrieval or in men with extremely low numbers of ejaculated sperm.
Intrauterine Insemination: IUI is a much simpler process that implants sperm further into the female reproductive tract and bypasses the cervix for improved odds of fertilization. It is used only rarely with surgically retrieved sperm but is an option in a few select cases.
Sperm Retrieval Options
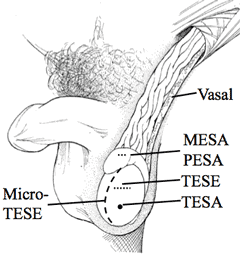
Testicular Sperm Extraction (TESA, TESE)
For these procedures, Dr. Turek removes immature sperm from the testicles. Testicular fine needle aspiration (TESA) is a nonsurgical technique that uses a needle to puncture the skin and testis to extract sperm in a minimally invasive manner.
Testicular sperm extraction (TESE) requires small incisions on the testicle to collect tissue and sperm. Dr. Turek also performs the microTESE approach which uses an operating microscope in more complex cases of testicular sperm retrieval.
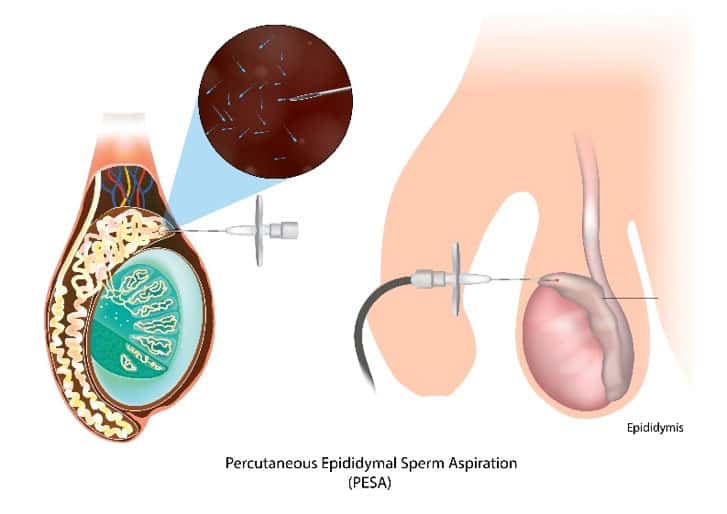
Epididymal Sperm Aspiration (MESA, PESA)
The epididymis is a tubular organ near the back of the testicle that transports sperm. Two procedures are used to retrieve sperm from this tube: microsurgical epididymal sperm aspiration (MESA), which uses a surgical microscope and percutaneous epididymal sperm aspiration (PESA), which uses a needle to acquire sperm. Typically the MESA procedure is the more reliable procedure to get good quality sperm in good numbers for use.

Vasal Sperm Aspiration (PVSA, MVSA)
This is the only sperm retrieval process that gathers “mature” sperm cells found in the vas deferens. It is an appropriate option for men who have normal sperm production but have some kind of blockage or condition that impedes sperm transport from the testicle to the ejaculate.
Sperm is more mature in this sperm duct since it has already passed through the epididymis. In fact, this sperm is essentially ejaculated sperm that is not ejaculated. For this reason, this sperm can be used with IUI to fertilize an egg on its own.
With MVSA (microscopic vasal sperm aspiration), Dr. Turek makes a small incision in the scrotum to access the vas deferens. PVSA (percutaneous vasal sperm aspiration) is a similar procedure except that it uses a needle puncture in the skin.
Streamlining the Testicular Sperm Retrieval Procedure

Amidst concerns about the invasiveness of biopsies and the risk of permanently injuring the testis, Dr. Turek invented the technique. During a 45 minute in-office procedure, Dr. Turek can learn whether sperm are present in the testes, where they are, and how much sperm is present. This information is used to create a “map” that guides testicular sperm retrieval. Thanks to sperm mapping™, fewer and smaller biopsies are required to harvest enough sperm to be used for IVF or ICSI.
More importantly, Dr. Turek’s sperm mapping™ technique has produced more success than other techniques. Published studies have found that sperm mapping™ found sperm in up to 45% of men who previously came up empty with TESE procedures and one in three men who failed with microTESE procedures. That offers significant hope to men who believed they were out of options.
Contact The Turek Clinic
It’s no wonder that Dr. Turek is called the “Sperm Whisperer” by colleagues in the field. If you have viable sperm somewhere in your reproductive tract, Dr. Turek will identify it and safely procure it to be used with IUI, IVF or ICSI. To schedule a consultation with Dr. Turek, please contact The Turek Clinic today.









