Varicocele Causes, Symptoms, & Treatment

What Is a Varicocele?
A varicocele is like a varicose vein in the leg, except that the swollen, twisted vein develops in the scrotum. Although most varicoceles do not cause pain or produce other symptoms, they are known to interfere with fertility.
Fifteen percent of the general population has varicocele, and approximately 35 percent of men that Dr. Paul Turek evaluates for infertility have varicocele. Identifying and treating varicocele can have a tremendously positive effect on male fertility and may help you father the biological children you have always wanted. In fact, varicoceles are the most commonly found surgically correctable cause of male infertility. Dr. Turek championed the development of microsurgical varicocele treatment and has trained dozens of fellow surgeons in the technique.
What Causes Varicoceles?
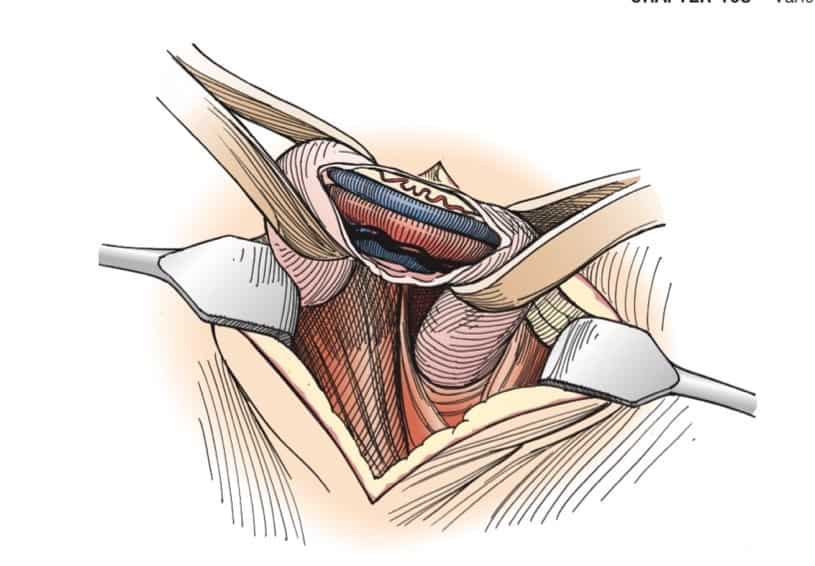
The testicles are suspended in the scrotum through the spermatic cord. Inside each cord is a tube that sperm travels through (the vas deferens), the testicular artery that pumps blood to the testicles, and a network of smaller veins called the pampiniform plexus that drain blood from the testicle into the testicular veins. A series of valves in the testicular veins prevent the blood exiting the testicles from flowing back into the testicles. Sometimes, these valves do not close completely or properly, and blood starts to flow backward due to gravity. This forms a varicocele, or enlargement of the veins. Varicoceles usually begin at puberty. Varicoceles often occur on the left testicle because the left testicular vein anatomy where it empties into the body near the kidney is subjected to the forces of gravity. The right testis is protected from the effects of gravity because of a natural “valve” on that side.
Does a Varicocele Have Symptoms?

A varicocele does not always have symptoms. In some cases, it may cause scrotal pain or discomfort, particularly after long periods of standing or physical activity. The pain may worsen throughout the day and lessen or disappear when laying down. Some varicoceles can enlarge, and cause a noticeable mass on the scrotum. Or a varicocele may cause the left testicle to look swollen or considerably bigger than the right testicle.
Do Varicoceles Affect Male Fertility?
We believe that excess warm blood in the scrotum comes down from the warmer body above it and causes the testes to overheat, interfering with their ability to make sperm and testosterone. The testicles hang in the scrotum away from the body because they must be slightly cooler than the body temperature to make sperm and testosterone. If something warms the testicles (like blood coming down from the body and pooling in the veins), it generally impairs sperm production.
Highly Effective Treatment for Varicoceles
You may have a varicocele, not know it and not have any symptoms or problems conceiving. In that scenario, you probably do not need to have it treated.
But if you are experiencing pain or fertility problems stemming from a varicocele, Dr. Turek may recommend a microsurgical varicocele repair procedure to close off the enlarged veins.
During the microsurgical procedure, a small incision is made in the upper scrotum and the spermatic cord is exposed. A small opening is made into the spermatic cord and the veins that make up the varicocele are tied with silk suture. The artery, lymphatic vessels and nerves are spared, and blood can still leave the testicles through other, smaller veins. The spermatic cord is restored to its bed and the incision is closed. The procedure takes less than one hour and is performed on a come-and-go basis. The complication rate is extremely low (<1 percent) and men are typically back to work and full activity within two to three days.
Dr. Turek is happy to answer your questions about varicoceles and their treatment during a one-on-one consultation at The Turek Clinic. Please contact us today to schedule an appointment.









