Sperm FNA Mapping: Looking Beyond the Conventional to Find New Hope for Infertile Men
How do you react when you are pinned against the wall by the unknown? Do you freeze? Succumb? Invigorate? I find that I get very calm and very creative. Going where no one’s been before feels atmospheric to me. And it’s where I do some of my best thinking.
Fertility from Sterility
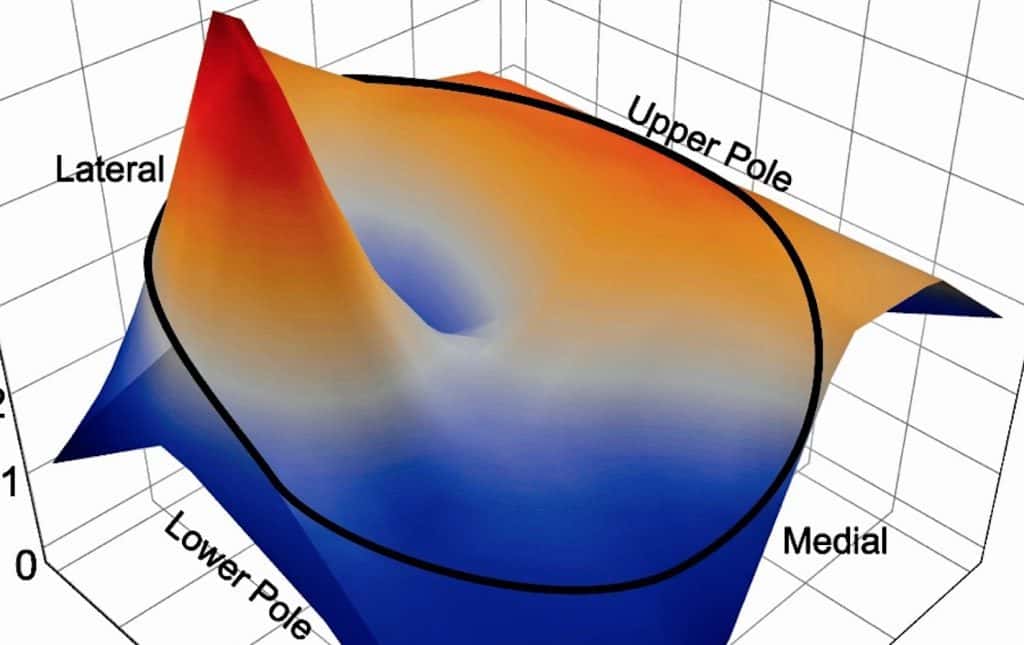
Two decades ago, the field of male infertility held two new truths: That men without sperm in the ejaculate can have sperm in the testicle, and that testicular sperm could be used to create babies with IVF-ICSI. We also learned that testicular sperm tends to be located in “islands” or “pockets” which means that it could be in one place but not another. A veritable hornet’s nest for the reproductive urologist.
One of the first “walls” I faced upon entering the field were patients who came to me after the traditional testis biopsy was unable to find sperm in the testicle, asking “is there anything you could do?” Thinking atmospherically, I invented Sperm Mapping™. Indeed, by looking harder and avoiding incisions, we published that Sperm Mapping™ was both kinder and better at finding sperm than the classic biopsy. And this was good.
Medieval vs Modern
At about the same time, and on the East coast, another solution to the “hidden sperm” problem was developed: microdissection testicular sperm extraction (micro-TESE). This is very different than Sperm Mapping™ in that it involves surgically bivalving the testicle, opening it like a book, after making a very large incision in its covering. By directly examining the testis tubules of the widely opened organ for several hours, surgeons using micro-TESE also found more sperm than the traditional biopsy could. But the consequences to the testicle, including pain and falling testosterone levels, were far more common after micro-TESE. Possibly due to the surgically heroic nature of the micro-TESE procedure, it became the favorite in the land. Until now.
Know Before You Go
Fast forward 15 years, and I began to see patients from around the world who had failed micro-TESE procedures, and they asked that same question: “Is there anything you could do to help us?” Against the wall again, I offered a now highly evolved version of Sperm Mapping™ to them. And guess what? I found sperm.
Of course, the devil is in the details and those can be found in our newly published study. Among a group of almost 600 sterile men from around who visited me over a 5-year period, 82 had had failed micro-TESE procedures. At an average of 2 years later, we “Mapped” these men and found sperm in almost 1/3 (29%) of cases – all of which were thought to be untreatable. Here are some other findings from the study:
- Among the men with sperm found on Sperm Mapping™ after failed micro-TESE and who proceeded to sperm retrieval yet again, sperm for IVF-ICSI were found in all patients.
- We banked extra sperm in 2/3 of cases of these salvage sperm retrievals. This means more kids later on without more surgery.
- Notably, the classic “look” of testis tubules required for micro-TESE success was not necessary for us to find sperm with Sperm Mapping™. It’s different when you “know before you go.”
Maybe it’s really true that good things come to those who wait. And who persist. Now there’s new hope for men who have failed all conventional attempts to find sperm. For me, it’s best summed up by Duke Ellington: “A problem is a chance for you to do your best.”