The Safety of Sperm Mapping
Hard to believe, but Sperm Mapping has its sceptics. Generally, they are few in number and they have never actually used the technique, but for some reason they appear wedded to the status quo. The basis of Sperm Mapping is fine needle aspiration (FNA), a tool that has been used in medicine for over 100 years. Tried and true, FNA gained popularity in the mid-20th Century in Sweden, where many of the world’s best practitioners learned the art.
The Origin of Art
I was taught Sperm Mapping by the Swedish School. Dr Britt-Marie Ljung, a Stockholm native and Professor at UCSF, taught me everything I know. Her skill was legendary. She routinely performed FNA on children’s eyes that had tumors within them. In this way a diagnosis could be made without removing the eye. Brilliant!
Let’s Hear It
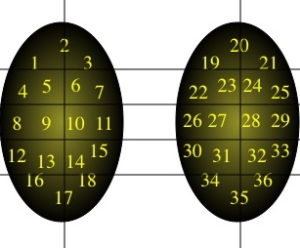
Some say that Sperm Mapping is “blind” when looking for sperm in the testicle. But a closer examination of Mapping would show that it’s a strategic and templated approach to finding sperm. When you lose your wallet at home, do you look for it in the park? No, you review where you’ve been and retrace your steps. Sperm Mapping is in no way blind but rather rigorously systematic in nature.
Some say it’s “risky” or even “dangerous.” In my experience and that of those I’ve trained in the technique, the overall risk is about 1/10 the risk of a simple blood draw (which is 10%). And the risk profile is no more serious than a blood draw. Also true is that Sperm Mapping risk is similar to that of FNA procedures performed elsewhere in the body (e.g. lung, liver, spleen, muscle, kidney, breast, thyroid, lymph node) over the past century. In other words, very, very low.
I’ve heard detractors say that it has to be unsafe, otherwise it would be far more popular than it is. To me, the reason why all surgeons don’t do Sperm Mapping is because (a) it requires learning a new skill and (b) it holds them to a higher standard of performance. Regarding skill, it appears that many doctors either don’t have what it takes or don’t care to learn the skill. Sorry, but I can’t help them either way. Better off that they don’t do Sperm Mapping.
When it comes to achieving high standards, the quality of every single Sperm Mapping sample is judged and graded. This, of course, sets a very high standard. It’s similar to telling a patient with cancer, “I’m positive that I can cure you” rather than the typical “Let’s see if I can cure you.” I love to be judged. It leads to constant improvement.
The Thing Speaks for Itself
How do I know Sperm Mapping is safe? I have followed the recovery of 1,000 men using a digital house call service (GetWellLoop) that connects us daily for 3 weeks after their procedures. As you can imagine, this intense connectivity provides enormous data on recovery. And from this, I can confidently state that there is simply no complication rate with Sperm Mapping. To boot, when sperm retrievals are done after Mapping, the testes appear in pristine condition, like nothing ever happened. Lastly, the ability to find sperm during sperm retrieval after Sperm Mapping ranges from 92-100%, which would be impossible if there were significant “damage” to the testicle! I invite my patients to chime in here if I misspeak!
Some say that Sperm Mapping is an unnecessary “extra step” in sperm retrieval. It turns a single- stage process into two steps. Well, GPS is unnecessary too, but do you use it to go somewhere you’ve never been? If you do, then maybe you understand the value of “knowing before you go,” which is the whole premise behind Sperm Mapping. It makes the later sperm retrieval more precise, faster, less invasive and twice as successful as an otherwise “blind” sperm retrieval.
So, for you disbelievers, realize that Sperm Mapping is an intentional, highly engineered and quality-controlled procedure that is backed by science, data, and two decades of clinical experience. Shallow, off-the-shoulder arguments to this hold no water.









