Failed Vasectomy Reversal in Los Angeles & San Francisco, CA

The ultimate measure of success in vasectomy reversal surgery is a pregnancy. There are several reasons why vasectomy reversals fail to achieve this goal and these are outlined here.
Reasons Why Vasectomy Reversals Fail
1. A pregnancy involves two partners. Although the count and quality of sperm may be high after vasectomy reversal surgery, female fertility factors may play an indirect role in pregnancy success and the reason for failure. Dr. Turek recommends that female partners age >35 years old consider a female factor evaluation to determine if they have adequate reproductive potential before a vasectomy reversal is undertaken. This evaluation can be done by a gynecologist and should include a cycle day 3 FSH and estradiol levels, AMH levels, an assessment of menstrual cycle regularity, and a hysterosalpingogram to evaluate for fibroids. Advanced maternal age is a common reason for vasectomy reversal failure.
2. A man without prior paternity before vasectomy may have abnormal sperm quality before the vasectomy. This could be a reason why semen quality after vasectomy reversal surgery is low and a reason for pregnancy failure. A physical examination and a blood test before the vasectomy reversal can inform Dr. Turek of the possibility that impaired sperm production is present and eliminate this reason for failure.
3. Approximately 30%-60% of men with vasectomies develop a reaction against their sperm (i.e.antisperm antibodies). High levels of these proteins directed against sperm may impair fertility, either by making it hard for sperm to swim to the egg or by interrupting the way the sperm must interact with the egg. Sperm bound antibodies can be a reason for vasectomy reversal failure and are usually assessed >6 months after the vasectomy reversal if no pregnancy has ensued. Treatment options include steroid treatment, intrauterine insemination (IUI) and in vitro fertilization (IVF) techniques.
4. Occasionally, scar tissue develops at the site where the vas deferens is reconnected, causing a blockage. In Dr. Turek’s vasectomy reversal procedure, this occurs in 5% of vasovasostomies and up to 15% of epididymovasostomies. Depending on when it occurs, it can be a reason for failure to achieve a pregnancy. It may be treated with anti-inflammatory medication or could necessitate repeat vasectomy reversal surgery.
5. If an epididymal blowout has occurred and is not discovered at the time of vasectomy reversal surgery, the vasectomy reversal will likely fail. In this case, an epididymovasostomy would need to be performed.
6. In certain patients, when the vas deferens has been blocked for a long time, the epididymis is adversely affected. Remember, sperm are nurtured to maturity within the normal epididymis. In these individuals, sperm counts may be normal, but sperm movement may be poor after vasectomy reversal. This is why Dr. Turek recommends antioxidants vitamins (A, C and E) or other supplements after vasectomy reversal surgery. Most patients will gradually recover from epididymal dysfunction. Those patients whose sperm continue to have problems may require IVF to achieve a pregnancy.
Challenges of Vasectomy Reversal Surgery
To better understand what makes vasectomy reversals challenging, a quick review of anatomy and physiology is helpful. Sperm are produced in the male sex gland or testicle. From here they exit the testes (efferent ductules) and enter a “storage site” or epididymis. The epididymis is essentially a single, 18 foot long, tightly coiled, small tube, within which sperm mature so that they can move, swim and fertilize eggs. Testicular sperm are not able to fertilize eggs naturally (but can if they are injected directly into the egg in the laboratory), as this is learned in the epididymis. From the epididymis, a 14 inch muscular tube called the vas deferens carries the sperm to the urethra near the base of the penis. The urethra then carries the sperm through the penis during ejaculation. A vasectomy interrupts sperm flow within the vas deferens. After a vasectomy, the testes still make sperm, but because the exit is blocked, the sperm die and are reabsorbed by the body.
Epididymal Blowout
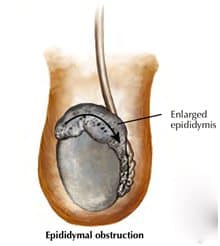
One issue that makes a vasectomy reversal challenging is that a problem can develop in the delicate tubes of epididymis over time after vasectomy. The longer the time since vasectomy, the greater the “back-pressure” behind the vasectomy. This “back-pressure” may cause a “blowout” in the delicate epididymal tubule, the weakest point in the system. The blowout may or may not cause symptoms, but will likely scar off the epididymal tubule, thus blocking sperm flow at a second point. To summarize, a man with a vasectomy can develop a second obstruction deeper in the reproductive tract that can make the vasectomy more challenging to reverse. Having the skill to detect and fix this difficult problem during vasectomy reversal is the essence of a great urologic microsurgeon.
In Dr. Turek’s practice, 40% of men seeking vasectomy reversal have this obstruction and 25% of his cases are patients who are previous vasectomy reversal failures by other surgeons. Dr. Turek is also comfortable tackling the technically challenging cases of traumatic, infectious or congenital blockages that require microsurgery.
If the surgeon simply reconnects the vas deferens without examining for a second, deeper obstruction, then the vasectomy reversal procedure can fail, as sperm will not be able to flow out of the “corrected” system. With epididymal obstruction, the vas deferens must be connected to the epididymis in front of the this blockage, to bypass both blockages and allow the sperm to reenter the urethra and ejaculate. Since the epididymal tubule is much smaller (0.3 mm diameter) than the vas deferens (3mm diameter, 10 fold larger), epididymal surgery is far more complicated, challenging and precise than the simple vas-to-vas connection and should only be undertaken by an experienced, skilled microsurgeon who performs them routinely.









