Hormone Replacement Therapy (HRT) for Men in Los Angeles & San Francisco, CA
The average age of men in the US is projected to rise significantly over the next 25 years, with the greatest increase occurring in men > 65 years old.
As this happens, there will be a dramatic increase in age-related health problems too, including cancer, strokes, heart disease and hormone deficiency. Although the health risks associated with age-related hormonal decline in women, termed menopause, have been thoroughly addressed, it has now been shown that hormonal changes in the aging male are associated with significant health problems.

Board-certified men’s sexual health expert Dr. Paul Turek has been named one of the “Best Doctors in America” for nine years running due to his extensive work with male hormone replacement therapy, among other fertility treatments. He has expertise in helping patients understand the issues that surround testosterone replacement therapy in men of all ages.
To learn more about HRT for men, schedule a consultation with Dr. Turek at The Turek Clinic in Beverly Hills and San Francisco.
Testosterone & Age

There is a progressive decline in testosterone production in men with age. These changes can be dramatic, such that 50% of men >60 years old have low levels of testosterone. Although the rate of decline varies widely, a general rule of thumb is that testosterone levels decrease about 1% yearly after age 50. Despite the fact that it is not as rapid a drop in hormones as women get with menopause, it certainly is just as real. This has been termed male menopause, male climacteric, andropause, or more appropriately, partial androgen deficiency in the aging male (PADAM). Serum testosterone levels in men fall progressively from the third decade to the end of life, mainly due to a decline in the cells in the testis that make the hormone (Leydig cells). This decline may also be due to changes in hormones (GnRH, LH) and proteins (SHBG, albumin) that regulate testosterone production.
Normal Testosterone Levels
One issue with testosterone that complicates matters is the fact that it exists in several different forms in the blood, and each form has different hormonal activity (Figure 1). “Free” or unbound testosterone is a fully active hormone, but protein-bound testosterone are only partly active, or sometimes completely inactive. What is usually measured in a blood draw is the total testosterone, which is a combination of the free and protein-bound forms. An analogy to explain this is to think of the total testosterone as all of the cars in a parking lot.
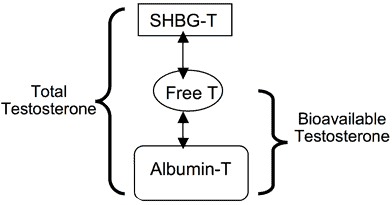
Importantly, though, only the cars that can start or drive are useful or active. Free testosterone comprises all of the cars that can start and be driven away, but the protein-bound testosterone are those cars that may or may not start, and those that may or may not be able to be driven away. So, aging is associated with 1) lower total testosterone production (fewer cars in the lot) and 2) higher levels of certain proteins that bind testosterone (sex hormone-binding globulin, SHBG), such that even fewer cars can start and run, and it is this combination of events that leads to declining testosterone activity with age. Thus, the complex physiology of testosterone balance often clouds the interpretation of age-related declining levels of the hormone.
The Role of Testosterone in Men

Testosterone affects the function of many organs in the body (Table 1). In the brain, it influences libido or sex drive, male aggression, mood and thinking. Testosterone can improve verbal memory and visual-spatial skills. It as also been shown to decrease fatigue and depression in men with low levels. It is responsible for muscle strength and growth, and stimulates stem cells and blood cells in bones and kidneys. Penile growth, erections, sperm production, and prostatic growth and function all depend on testosterone. It also causes body hair growth, balding, and drives beard growth. Thus, testosterone makes us who we are, and influences how we look.
Table 1. Testosterone effects in the normal Male.
Advantages of Testosterone Replacement Therapy
Better Bones

In men with low testosterone levels, testosterone can improve bone mineral density and reduce bone fractures, an effect similar to that found in postmenopausal women on estrogen replacement. Importantly, hip fractures are 2-3 times as likely to kill an older man as a woman of the same age, and 40% of older male patients with hip fractures die within 1 year of the injury.
Leaner Body
Testosterone results in increases in lean body mass, possibly strength and can decrease fat mass. By stimulating erythropoietin, testosterone increases blood counts. It appears to improve lipid profiles and dilates blood vessels in the heart but no data has yet shown that it reduces heart attacks or strokes. It appears not to alter LDL or total cholesterol levels. In recent work, it has been shown that men with chronically low testosterone levels have 2-3 fold higher risk of developing metabolic syndrome and have up to a 40% greater risk of death than men with normal testosterone levels.
Better Sexual Health
Sexual function also improves with testosterone. Most studies agree that sexual drive is improved by testosterone. Penile erections may be improved with testosterone, but only in men with low testosterone levels. Important, isolated low testosterone is an unusual (6%) cause of erectile problems in older men as lower sex drive and age-related changes to the penis are far more common.
Low Testosterone Symptoms & Diagnosis
To make an accurate diagnosis of low testosterone, symptoms or findings must accompany a blood draw showing a low testosterone level. This combination makes treatment worthwhile to pursue. Symptoms include decreased sexual desire and erectile dysfunction, changes in mood associated with fatigue, depression and anger, and decreases in memory and spatial orientation ability. On examination, there may be decreased lean body mass with reduced muscle volume and strength, and increases in abdominal girth. Decreased or thinning of facial and chest hair and skin alterations such as increases in facial wrinkling and pale-appearing skin suggestive of anemia may also be noted. Testicles that have become smaller or softer may also be present. Finally, low bone mineral density with osteopenia or osteoporosis may also suggest a problem.
Not all of these findings need to be present at the same time to diagnose the problem. In fact, many of these symptoms can be attributed simply to the natural and unavoidable consequence of aging. For example, frailty may be due to many causes, some of which include loss of muscle strength, bone fractures, decreased mood, and impaired cognition, symptoms typical of testosterone deficiency. However, the association of such symptoms along with a low testosterone certainly implicates this as a problem. By these criteria, it is estimated that only 10% of men with low testosterone levels are currently being diagnosed.
Laboratory Tests
Because testosterone is found in several forms in the blood, there is debate as to what test is best to diagnose testosterone deficiency. In general, a total testosterone is ordered first. Dr. Turek then follows the algorithm in Figure 2.
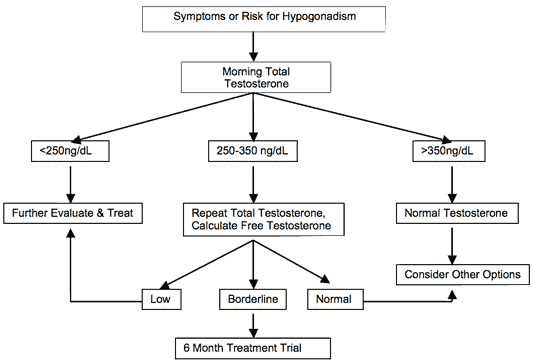
National guidelines suggest that a testosterone level below 300 ng/dL is suspicious for being low, but obviously this will vary among men. Evidence of a prior testosterone level that is much higher than a current level might warrant treatment even if the current level is > 300ng/dL. Presently, measuring testosterone byproducts such as dihydrotestosterone (DHT), estradiol and dihydroandrosteindione (DHEA) is not that useful in making the diagnosis.
Other Tests
Although not used in all cases, a blood count showing anemia may help make the diagnosis. In addition, a DEXA scan is an accurate, quick and painless procedure for measuring bone density or bone loss. The amount of radiation used for this X-ray technique is extremely small – less than 1/10 the dose of a standard chest x-ray. Bone density assessments can also be performed periodically during testosterone replacement to assess the bone response to treatment. Certainly an evaluation for prostate cancer with a PSA and rectal examination is indicated in men who are at risk prior to testosterone treatment.
Replacement Therapy for Low T
The ideal testosterone therapy maintains normal concentrations of the hormone without having significant side effects. Several kinds of hormone replacement are currently available at The Turek Clinic, including oral, injectable, transdermal and buccal mucosal systems as outlined in Table 2.
Table 2. Types of testosterone therapy in the US.
| Preparation | Forumla | Dose | Specific risk/benefit |
|---|---|---|---|
| Oral | Methyltestosterone Fluoxymesterone | 10-50mg/day | Multiple daily doses. Risk of liver problems |
| Intramuscular | Testosterone cypionate Testosterone enanthate | Testosterone cypionate Testosterone enanthate | Deep intramuscular injection. Gives very high and low levels; mood fluctuations. No daily regimen. |
| Subdermal implant | Testopel | 5-10 gms | Nonsurgical procedure to place implant. Migration. Lasts 3-6 months |
| Transdermal patch | Testoderm (scrotal) Testoderm TTS Androderm | 4-6mg/day 5mg/day 2.5-5mg/day | Scrotal patch: daily shaving, variable abpsorption. Non scrotal patch: skin welts at patch site. |
| Transdermal gel | Androgel Testim | Androgel Testim | Rubs off on partner or children. Odor. High convenience factor. |
| Transbuccal pill | Striant | 30mg buccal tablet | Take twice daily. Gum or mouth irritation. Taste perversion. |
The most popular choices are the transdermal gels (70% of patients), injectables (17%) and then transdermal patches (10%).
Monitoring of Testosterone Therapy
Testosterone replacement is generally considered a long term therapy and patients need to be monitored regularly as outlined in Table 3. Prior to starting treatment, a digital rectal examination and serum PSA are important. Within a month or two after treatment is started, symptoms and testosterone levels should be assessed. During the first year of therapy, patients should be followed regularly to assess clinical response. After the first year, patients who are stable may be followed annually. Annual evaluations should include testosterone, hemoglobin, liver function tests, lipid profile and PSA tests. Bone density and psychological evaluations can be done depending on the original reasons for treatment.
Table 3. Monitoring before and during testosterone treatment.
| Time | Indicated Assessment |
|---|---|
| Baseline (Pre-treatment) | Blood counts (hematocrit) and PSA. Rectal exam (prostate cancer). Ascertain voiding symptoms, sleep apnea. Consider DEXA scan for bone mineral density. |
| 1-2 months of treatment | Assess efficacy: testosterone level and symptoms. Adjust dose for either variable. |
| 3-6 month intervals during 1st year | Assess symptomatic response, voiding symptoms and sleep apnea. Physical exam, rectal exam, testosterone, liver and lipid profile, PSA, and hematocrit (depending on formulation). |
| Annually after 1st year | Assess symptomatic response to treatment, voiding symptoms and sleep apnea. Physical and rectal exam; testosterone, liver and lipid profile, PSA, and hematocrit (depending on formulation). |
Alternative Treatment Options to Testosterone Therapy
Dihydrotestosterone (DHT)
The natural androgen DHT is a metabolite of testosterone. It is a selective androgen because, unlike testosterone, it cannot be converted to estrogens. It is also a potent androgen, binding to receptors more avidly than testosterone. DHT has an effect on several target tissues, including external genitalia, prostate and skin. DHT deficient men have normal muscle mass and are not osteoporotic. In normal men, DHT supplements suppress pituitary FSH and LH secretion, likely causing infertility. As an androgen, DHT is relatively “prostate sparing.” Because of its potency and potential, significant research is being conducted with DHT supplements for androgen replacement.
Dehydroepiandrosterone (DHEA)
DHEA is available in over-the-counter formulations in the US. It is a steroid hormone made by the adrenal gland and its level progressively declines beginning the third decade of life and beyond. As a consequence of this, studies have attempted to correlate levels of DHEA and DHEA-sulfate with many health conditions. Clinical trials looking at DHEA for multiple conditions have been inconsistent. Placebo-controlled studies suggest that doses of 30-50mg of oral DHEA may produce physiologic androgen levels. In men with poor adrenal function, 50mg of oral DHEA can increase serum androgen levels to within the physiologic range for young adults, improve sexual function, mood and self-esteem, and decrease fatigue/exhaustion. However, its value in older men is not well established.
Growth Hormone
There are decreases in growth hormone and insulin-like growth factor-I with age in both men and women. In addition, treatment of young GH-deficient adults with growth hormone improves body composition, muscle strength, physical function, and bone density, and reduces blood cholesterol and cardiovascular disease risk. Some of these improvements are in health domains similar to those affected by testosterone. However, growth hormone treatment is often accompanied by carpal tunnel syndrome, peripheral swelling, joint pain and swelling, breast tenderness, glucose intolerance, and possibly increased cancer risk. In older individuals, growth hormone treatment improves lean body mass and reduces body fat. However, clinically significant functional benefits, prolongation of youth, and life extension have not been demonstrated. Until more research better defines these risk/benefit relationships, treatment of elderly individuals with growth hormone is not recommended.
Risks and Side Effects of Testosterone Therapy
The general risks of testosterone replacement are:
Water retention
This may lead to hypertension, leg swelling, or worsening heart failure. Weight and blood pressure monitoring are important for at-risk patients on therapy.
Infertility
Testosterone therapy of any type generally leads reduced sperm production. In fact, zero sperm counts occur in 90% of patients within 10 weeks of starting therapy. Sperm counts usually rebound within 6-12 months after therapy is stopped. Patients on testosterone should be informed that fertility will be impaired during treatment.
Excessive red blood cell count
Excessive red blood cell count (polycythemia) was a commonly observed side effect in a meta-analysis of clinical trials of testosterone therapy. Blood counts (hematocrit) levels above 50 have been associated with an increased risk of stroke. Polycythemia is most commonly seen with injectable testosterone. Monitoring blood counts is important for patients on testosterone replacement. In addition, testosterone may suppress clotting factors II, V, and VII, and worsen bleeding in patients on anticoagulation.
Liver damage
Liver damage has been reported with oral treatments. However, it is very rarely observed with injectable, transdermal and transbuccal formulations.
Sleep apnea
Although it does not cause sleep apnea, testosterone therapy can worsen existing sleep apnea. Men at risk of sleep apnea include elderly and obese men, and those with chronic obstructive pulmonary disease.
Breast tenderness
Painful breast enlargement (gynecomastia) due to high levels of estrogen (which comes from testosterone) can develop during therapy. Medications call estrogen receptor blockers can treat this side effect.
Altered cholesterol balance
Testosterone therapy is not thought to affect total cholesterol or LDL cholesterol, but the affect on high-density lipoprotein (HDL) levels remains unclear. It is reasonable to follow lipid levels during treatment.
Prostate health
One of the most concerning risks of androgen replacement is the potential to worsen detected or undetected prostate cancer. However, no link has been made to testosterone replacement and the development of prostate cancer. Careful follow-up of patients at risk for prostate cancer while on testosterone therapy is important. The FDA recommends that testosterone therapy not be given to men with prostate or breast cancer. A second concern is whether testosterone treatment worsens urinary symptoms in men with enlarged prostates. For this reason, voiding symptoms should be monitored in treated patients.
References:
- Turek PJ. Smith’s Urology, 17th ed. Edited by EA Tanagho and JC McAninch. Appleton and Lange, Stamford, 2003. Chapter 46.