Invagination Epididymovasostomy During Vasectomy Reversal
Rajveer S. Purohit and Paul Turek MD
Department of Urology, University of California, San Francisco
San Francisco, Californnia
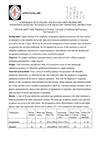
The field of urologic microsurgery has witnessed major advances in the past several years. This is no more evident than with epididymovasostomy surgery, performed for male reproductive tract obstruction. The most common reason for epididymal obstruction is vasectomy. Among the 500,000 vasectomies performed in the US annually, 2-5% of men will seek reversal. Although patients initially harbor only a single site of obstruction in the vas deferens, risk of a secondary epididymal obstruction increases with time after vasectomy. Other causes of epididymal obstruction include trauma, epididymitis, Young’s syndrome, congenital anomalies, ejaculatory duct obstruction and the secondary effects over time due to vasal obstruction during hernia repair.
“…among the 500,000 vasectomies performed in the US annually, 2-5% of men will seek reversal.”
– Dr. Paul Turek
The history of epididymovasostomy surgery is interesting. Before the era of the operating microscope (pre-WWII), early urologists attempted to connect the vas deferens to the epididymis with procedures that encouraged fistula formation rather than attempting a direct anastomosis. In 1978, Silber first reported the microscopic approximation of the vasal mucosa directly to a single epididymal tubule in an end to end manner (1). The next major advance was the vasal end to epididymal tubule side epididymovasostomy as popularized by Thomas in 1987 (2). Although still technically challenging, this procedure was more widely accepted because the epididymal tubule was easier to identify and manipulate for a formal two-layer closure.
The most recent innovation, first described in 1991 (3, 4) and later popularized by Berger (5) and Marmor (6), is termed the invagination epididymovasostomy. The essential difference between this technique and the prior end-to-side epididymovasostomy involves the inner layer of the two-layer microsurgical anastomosis. Instead of performing a formal mucosa-to-mucosa anastomosis of vas deferens lumen to an epididymal tubule, there is intussusception of a loop of epididymal tubule into the vasal lumen. This approach uses fewer sutures yet promises a more leak-free anastomosis than the mucosa-to-mucosa approach. The specifics of this technique are reviewed here.