Testis or Testicular Biopsy
A testis biopsy is helpful in many cases of azoospermia. If an evaluation of azoospermia is not clearly showing whether there is a problem with sperm production or one of a blockage in the ducts of the reproductive tract, then the next step is to examine the testis itself and assess sperm production.
This can be done in several ways, but the classic approach is to perform a testis biopsy under local anesthesia. This allows for the direct inspection of a small piece of testis tissue to determine whether sperm production is normal or not. Testicular tissue contains
- sperm-producing cells that are found in tubules called seminiferous tubules, and
- cells between the tubules that are called interstitial or Leydig cells.
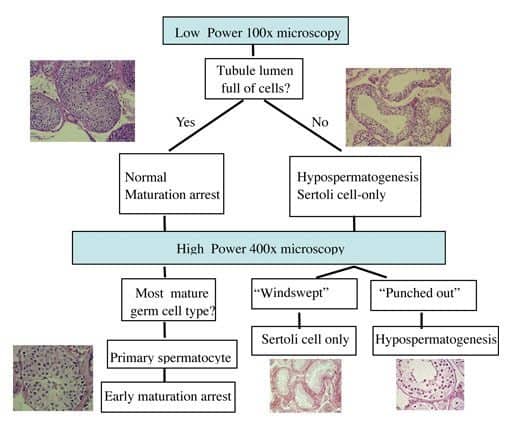
The Leydig cells are the major hormone-producing cells. The biopsied tissue is specially stained and examined microscopically for both cell types by a pathologist. If it shows that sperm production is normal, then a blockage exists in the system, usually beyond the testis. Remember that a biopsy does not tell us where the obstruction is located within the system. The most common testis biopsy patterns observed in a testis biopsy specimen are listed below. Dr Turek has created a systematic way to interpret the testis biopsy that he has taught others for years to decide what pattern is present (see figure below).
Testis Biopsy Patterns
Normal
The testis architecture and sperm production look entirely normal. This means that an absence of sperm in the ejaculate is due to an obstruction or absence of the ducts leading from the testicle to the penis.
Maturation Arrest
Sperm are made from early germ cells that develop within the testicle. The process of sperm maturation can be interrupted at several levels and can result in several “arrest” patterns. If the halt in development occurs early in the process of sperm maturation, the prognosis is worse.
Hypospermatogenesis
In this pattern, all of the elements of sperm production are present, but there are fewer of them than normal. This will generally result in lower numbers of sperm in the ejaculate.
Germ Cell Absence or Aplasia
This pattern occurs when there is no sperm found in the testicular biopsy. When there is no definite reason for this lack of germ cells and sperm, it can also be termed ‘Sertoli Cell-Only Syndrome’.
Other
Other abnormalities can be detected by examining a testis biopsy, including evidence of previous infection within the testis and abnormalities of the Leydig or interstitial cells. Occasionally, testis cancer can be detected, but this is a rare (less than 1%) finding in the U.S.
In Dr. Turek’s experience, the testis biopsy has several limitations. For one, it is invasive. Second, it only provides information on the area that is biopsied and tells us nothing about sperm production in the rest of the testis. Third, how clinicians read the biopsies varies widely, making the interpretation unclear, a fact that does not help the patient. In fact, Dr Turek has published on this issue of how testis biopsy interpretations vary in a series of testis biopsies from patients who had had the biopsy procedure done before they consulted with him. In this study, he compared his interpretation of the biopsies from patients to the readings made by the pathologists from the community in which the biopsies were performed. He found that in 40% of cases, the interpretation that he made was different from the pathologist’s interpretation and that in 25% of cases, patient care was altered dramatically as a result of his re-review. An example of a significant alteration in care is a biopsy in which the community pathologist read as having no sperm but Dr. Turek’s reading suggested that there were sperm. For these reasons, the testis biopsy currently plays a limited role in the cutting edge care of azoospermic men. In addition, this is why Dr. Turek offers to re-review the testis biopsy slides that are sent to him as part of his Second Opinion Clinic.
Testicular Biopsy Results Interpretation
Testis Biopsy Alternatives
Because of the recognized limitations of the testis biopsy, about 15 years ago Dr. Turek pioneered a nonsurgical, less invasive alternative to the testis biopsy that is termed fine needle aspiration (FNA) “mapping” for men with azoospermia. FNA mapping is also known as sperm mapping™ or testicular mapping. He has performed over 1200 cases and testicular mapping is now popular throughout the world. More about testicular mapping.
Schedule a Testicular Biopsy Consultation
If you have recently been diagnosed with azoospermia and would like to learn more about the testicular biopsy procedure, schedule an appointment with Dr. Paul Turek at The Turek Clinic. Offices located in Los Angeles and San Francisco.
References:
- Cooperberg MR, Chi T, Jad A, Cha I, and PJ Turek. Fertil Steril 2005; 84: 672-7.









