Varicocele Repair in Los Angeles & San Francisco

Relieve Discomfort and Improve Fertility Problems with Varicocele Repair
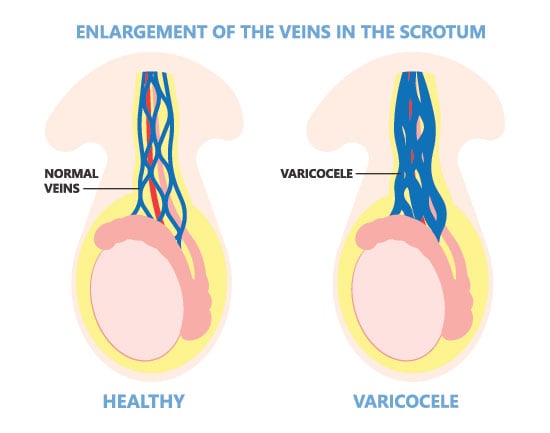
Varicocele is a network of abnormally large veins in the scrotum. It is thought to occur when the valves in the testicular vein malfunction, causing blood to collect in the scrotum. This abnormality can cause persistent discomfort and in some cases, impair male fertility. Dr. Paul Turek has discovered varicocele in approximately one-third of men that he evaluates for fertility-related problems. Although the exact mechanism by which varicocele affects fertility is unknown, Dr. Turek and other experts believe that the collection of blood in the scrotum causes the testes to overheat and interrupts their ability to make sperm and testosterone. The objective of varicocele treatment is to “cool off” the testicles by stopping the backward flow of blood from the body to the scrotum. Evidence suggests that repairing a varicocele can improve testicular function and help men go on to father biological children.
Varicoceles Overview
Approximately 10-15% of men have varicoceles, but varicoceles do not automatically translate to fertility issues. in fact, most men with varicoceles are fertile. However, the American Society for Reproductive Medicine reports that 40% of men with fertility issues have a varicocele vein. Almost all cases of varicocele affect the left testicle, although 5% of men have bilateral varicoceles which means they are present in both the left and right testicles.
There is evidence to suggest that varicoceles can become more problematic for fertility with time. Boys usually develop varicoceles during puberty and the effects of these dilated veins act over time to reduce both sperm and testosterone production. This can result in good fertility in young adulthood but infertility in later adulthood. That is why Dr. Turek and fellow male fertility specialists commonly find (80%) varicoceles in men who have previously had a child but struggle to achieve a subsequent pregnancy.
As far as infertility goes, a scrotal varicocele is arguably one of the easiest to treat. In fact, it is the most common correctable cause of male infertility. Varicocelectomy is not a particularly difficult procedure for a patient to undergo, and the results tend to be both effective and durable. Many men who have this procedure go on to produce a pregnancy within the first year, though all patients’ fertility journeys are unique.
It is necessary to treat varicoceles since they do not go away on their own. About 75,000 men in the United States have varicocelectomy each year.
Symptoms of Varicoceles
Men often notice pain or discomfort in their scrotum, often described as a “dragging” feeling, toothache-like or a “heaviness” with varicoceles. This pain typically occurs after either sitting or standing for a long time, which can cause pressure to accumulate in the varicocele. Others note a soft, “doughy” sensitive mass (of veins) above or around the testicles with varicoceles.
However, many men who have a varicocele are not aware that they have this condition because they have no symptoms. In fact, they may not know they have one unless fertility problems arise. In cases where scrotal discomfort is significantly bothersome, treatment is warranted for varicoceles even if fertility is not an issue.
When to See Dr. Turek for Treatment
Not all varicoceles need to be treated. You may not know you have a varicocele, and may not experience any noticeable discomfort or pain from the abnormality.
On the other hand, if you have been diagnosed with a varicocele that could be interfering with your ability to father a biological child, affecting your testosterone levels or causing you scrotal pain or discomfort, you should seriously consider having it repaired.
Dr. Turek can discuss the procedure in detail with you during a personal consultation. Before suggesting varicocele repair, Dr. Turek will want to confirm there are no other obvious causes for male infertility (e.g., a genetic abnormality or an obstruction of the reproductive tract). Blood tests and semen analysis may be taken when deciding whether to recommend varicocele repair. If repaired for pain, Dr. Turek would want to confirm that the pain pattern fits with a varicocele and is not due to other causes.

A Minimally Invasive Solution to Varicocele
There are several ways to repair a varicocele. Dr. Turek prefers the microscopic subinguinal microsurgical approach to varicocele repair, as it offers the highest success rates with lowest complication rates. He helped to popularize this approach in the 1990s, and has since trained over 50 urology residents, fellows and practicing urologists in the technique. As a master microsurgeon, Dr. Turek’s complication rates are extremely low.
The varicocelectomy is a short outpatient procedure, performed under light general anesthesia along with local anesthesia. Total treatment time is approximately an hour. There is minimal post-operative pain that can be easily managed with either non-prescription or prescription medication. Most patients can resume work and day-to-day activities within two days.

Procedure Details
Varicocele repair involves interrupting or tying off the veins leading from the testis, leaving vasal veins intact to carry blood to the body.
To begin the procedure, Dr. Turek creates a small incision in the upper scrotum and exposes the spermatic cord. Using an operating microscope to help him visualize the area, he inspects it for abnormal veins that are feeding the varicocele. These veins are interrupted or tied off, while the artery and lymphatic vessels and nerves are spared.
After returning the spermatic cord to its bed, Dr. Turek closes the incision with two layers, placing steri-strips and a bandage.
Varicocele Repair Recovery
After your surgery, have a loved one drive you home. Focus on resting and relaxing for the first 24 hours. You should ice the area of the incision for the first 48 hours. Your scrotum may appear swollen and bruised for a week. During this time, you may notice some lingering discomfort, which can be managed with medication or ice packs. You can shower daily and get the small incision(s) wet. The bandage strips on your incision should fall off on their own within a week’s time.
Generally, you can return to work within a few days unless you have a physically demanding job. While walking is a good activity to increase your circulation, strenuous activity should be postponed for one week. Sex should also be postponed for 1 week. Sexual and other activity can be increased as you see fit after 1 week.
Varicocele Repair FAQ
How is varicocele diagnosed?
A physical examination by a healthcare professional is often sufficient for diagnosis. A doctor may ask the patient to stand and forcefully exhale to make the varicocele more prominent. In some cases, particularly for more subtle or bilateral varicoceles, an ultrasound may be necessary to confirm the presence and severity of a varicocele.
What are the symptoms of varicocele?
- Dull, aching pain: Typically felt in the scrotum, the pain may increase with prolonged standing or physical exertion and improve when lying down.
- Feeling of heaviness: A sensation of heaviness or dragging in the testicle, especially after physical activity or towards the end of the day.
- Visible or palpable enlarged veins: The affected veins in the scrotum might be visible or feel like a bag of worms, particularly noticeable when standing.
- Swelling in the scrotum: Increased swelling in the scrotum as the day progresses.
- Testicular atrophy: Shrinkage of the affected testicle, which might be smaller than the other.
- Impaired fertility: Potential impact on sperm production and function, which may lead to fertility issues.
Do varicoceles always require treatment?
Not always. Some varicoceles are asymptomatic and don’t require intervention. However, men who have symptoms or concerns that they have varicocele should always seek the advice of a men’s health specialist. Treatment is typically necessary for those experiencing significant discomfort, testicular atrophy, or infertility issues. Plus, patients should be aware that untreated varicoceles can progressively worsen, which can lead to further health complications. Therefore, careful monitoring and regular check-ups with a healthcare provider are essential if you have been diagnosed with varicocele.
How can I prevent varicoceles?
There is no definitive way to prevent varicoceles. However, maintaining a healthy lifestyle, including regular exercise and a balanced diet, may contribute to overall vascular health. Schedule regular medical check-ups with your physician to monitor and manage potential issues, including varicoceles. Early detection and intervention can help mitigate potential complications and ensure long-term reproductive health.
Are varicoceles more common on one side of the scrotum?

Yes, varicoceles are significantly more common on the left side of the scrotum. This is due to anatomical differences in the venous drainage system, with the left testicular vein draining into the left renal vein at a right angle, which can lead to increased pressure and pooling of blood.
Right-sided varicoceles, which are rare, are often associated with other medical conditions. For instance, a unilateral right varicocele can indicate a potential obstruction or compression in the venous system, such as a tumor or other mass. This makes it important for individuals with a right-sided varicocele to undergo further medical evaluation to rule out any underlying conditions.
Can a varicocele lead to other medical conditions ?
While varicoceles primarily affect reproductive health, they can also lead to secondary conditions:
- Testicular atrophy: Prolonged varicoceles can result in testicular shrinkage, potentially impacting hormonal balance and fertility.
- Hydrocele formation: Fluid accumulation around the testicle, leading to swelling and discomfort, can occur either due to the varicocele itself or as a complication of treatment.
- Chronic pain: Many patients first discover they have varicocele because of the testicular pain they are experiencing. This includes young patients. Dr. Turek often treats young boys for varicocele to stop this pain and avoid fertility issues later in life.
Can I still father a child if I have a varicocele?
Yes, it is possible to father a child even if you have a varicocele. While varicoceles can impact fertility by reducing sperm count, motility, and morphology, many men with varicoceles still conceive naturally. Of course, seeking treatment for varicocele can dramatically improve your likelihood of conceiving a child. Additionally, assisted reproductive technologies like intrauterine insemination (IUI) can also provide options for couples facing fertility challenges due to varicoceles.
Contact The Turek Clinic
One of the nation’s foremost male infertility specialists, Dr. Turek helped to popularize the minimally invasive varicocelectomy procedure that has become so common today. If you are concerned that a varicocele is preventing you or your partner from fertilization, please schedule a consultation by calling 1-888-887-3563.









